“Azure’s International AZ Awards recognize excellence and innovation in architecture and design, and celebrate the world’s best projects, products and ideas.”

This international design competition annually selects winners in the categories of design, architecture, landscape architecture, urban design, experiential graphic design, interiors, concepts, student work and social good/environmental leadership. The 2022 awards saw Toronto’s Mirvish Village redevelopment project winning in the Urban Design Vision category. Click here to read more about the Mirvish Village AZ Award.
Award-winning Redevelopment
Mirvish Village is rising on the site of ‘Honest Ed’s,’ a much-loved discount store that was at the heart of Toronto’s Mirvish Village neighbourhood for almost 70 years. The redevelopment is currently under construction and spans 4.5 acres, creating nearly 1 million ft2 of purpose-built rental housing and retail space.
Mirvish Village has a focus on sustainability and affordability. To achieve this, the redevelopment is incorporating a district energy system and micro-grid that will offer a resilient means of thermal energy, power, and emergency power, enabling the project to meet LEED platinum and the City of Toronto’s Tier 2 Toronto Green Standard requirements.
HH Angus’ Role
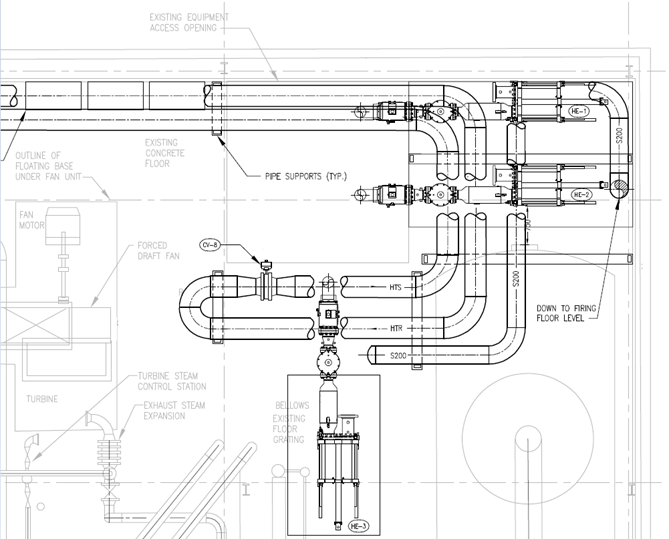
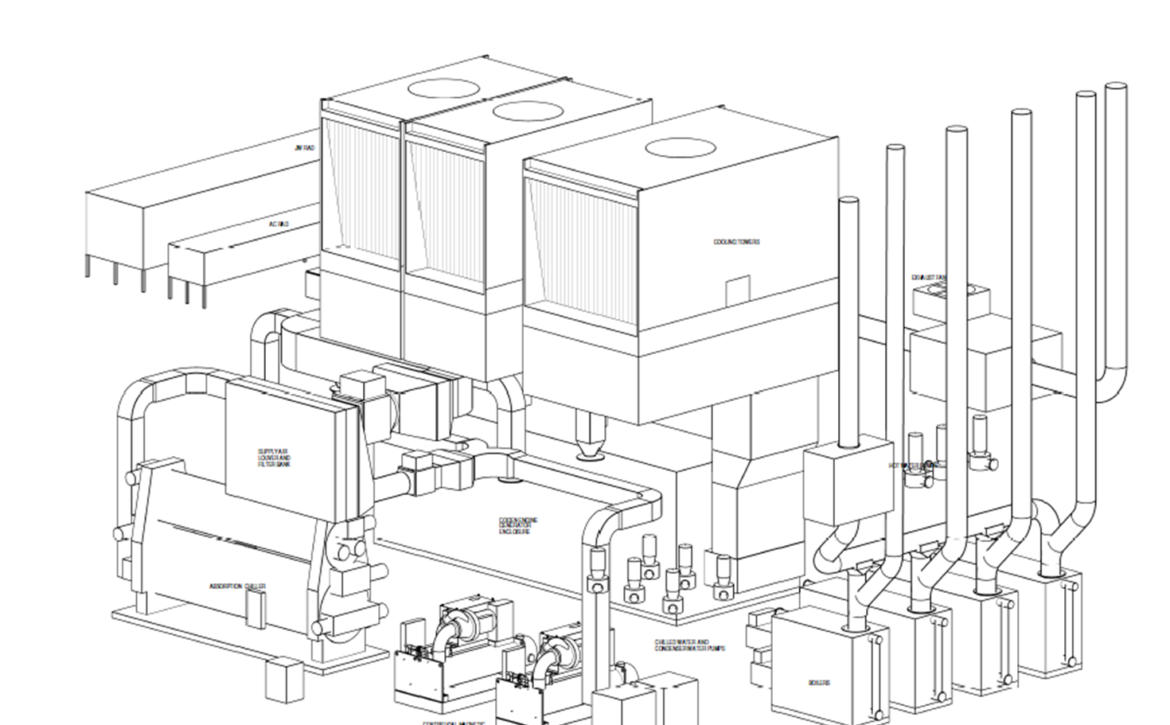
Our Energy Division team worked closely with Creative Energy Developments to provide mechanical and electrical engineering services for the Village’s central utility plant, which includes a combined heat and power plant (CHP), a boiler plant, and a cooling plant. The CHP plant includes an 800 KW generator set with auxiliaries and heat recovery system. The generator is expected to run continuously to provide power to the complex.
Heat recovery consists of two systems: high temperature to provide heat to buildings, and low temperature to provide additional heating for a winter snow melting system and swimming pool heating. The boiler plant includes four condensing hot water boilers, with the option for two additional boilers in future. All boilers have an output of 3.1 MW.
The cooling plant includes two water-cooled chillers, operating at 1200 tons each. One is a magnetic bearing chiller with variable frequency drive (VFD), and the other is a centrifugal chiller with VFD. As well, two rooftop cooling towers at 1200 tons each have been installed.
Central distribution piping from the plant will provide hot water and chilled water to multiple energy transfer stations, with heating, cooling, and domestic hot water heat exchanges for each building within the complex.
A photo-voltaic solar system will have a capacity of 103KW, 480V. HH Angus provided direction for locating the installation, coordinated with the PV supplier for modeling the panel direction and angle for optimal PV output, developed technical connection requirements with Toronto Hydro, and identified requirements for parallel generation with the central utility plant. Our scope also included developing thermal and electrical metering strategies within a microgrid system, and design of operation for gas-fired emergency generators in electrical peak shaving mode.
Rendering courtesy of Westbank Corp