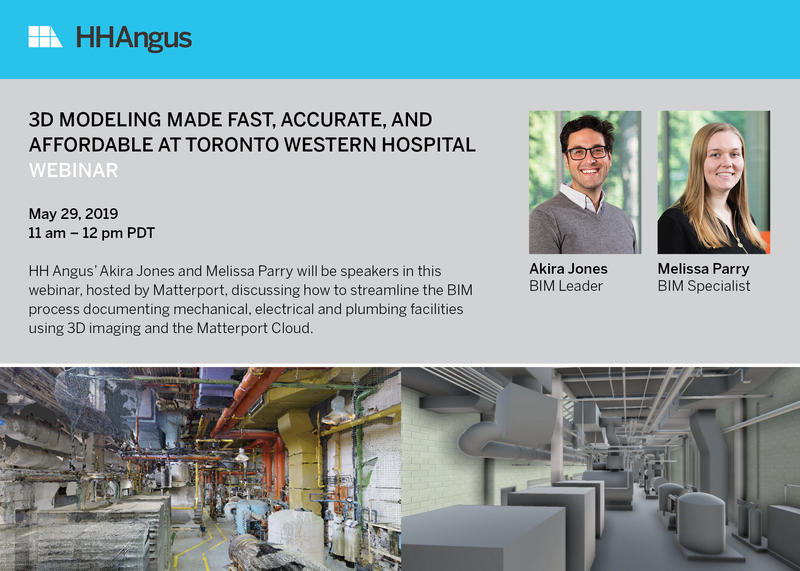
HH Angus' Akira Jones and Melissa Parry will be participating in a #Matterport webinar on May 29 discussing how we used 3D imaging to streamline the #BIM process for Toronto Western Hospital's mechanical and electrical facilities.
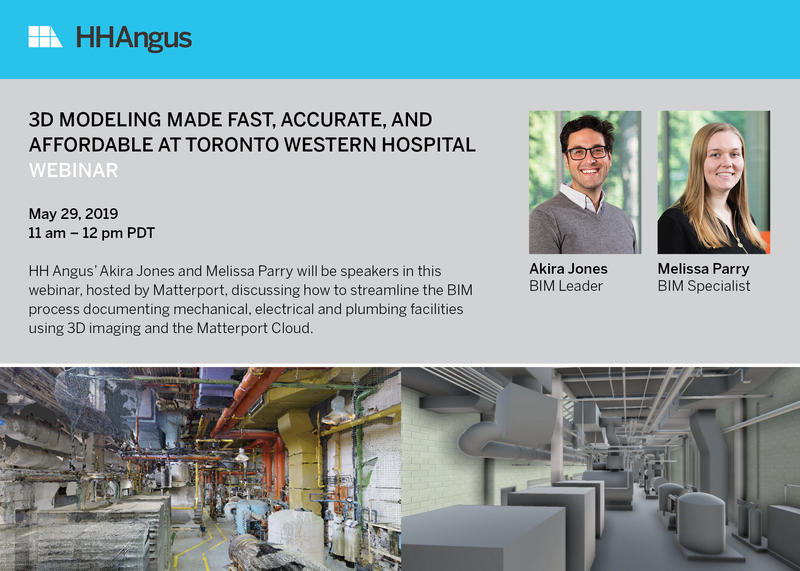
HH Angus' Akira Jones and Melissa Parry will be participating in a #Matterport webinar on May 29 discussing how we used 3D imaging to streamline the #BIM process for Toronto Western Hospital's mechanical and electrical facilities.

Join us in Montreal on Oct 16 as HH Angus presents “Making a Super Hospital Work” at the Canadian Centre for Healthcare Facilities conference.
As the mechanical, electrical and security design engineers for CHUM, the HH Angus team has unique insight into what it took to successfully deliver the largest healthcare project in North America – the Centre hospitalier de l’Université de Montréal. Nick Stark, Marianne Lee and Phil Schuyler, principals of HH Angus and team leaders, will detail some of the key challenges and solutions for this mega hospital project. Conference attendees will also be able to tour public, clinical, mechanical and electrical facilities at CHUM.

On January 13, Toronto’s Emerging Leader Forum (ELF) hosted an engaging discussion on Digital Health focused on informing young leaders in healthcare. The event was led by Dr. Darren Larsen, Chief Medical Information Officer at OntarioMD, who facilitated the discussion with:
Despite having a relatively straightforward label, the concept of digital health encompasses a complex set of ideas that differ greatly between sectors and people. While many associate digital health with smartphone apps and telehealth, Dr. Trevor Jamieson is quick to differentiate between virtual health and digital health, noting that “how you use data to drive better decision making” forms the core of how digital health impacts how we care for patients. Many would agree that data has become critical in the delivery of healthcare across varying sectors from acute to primary care, and the ability to manage and apply data efficiently will likely become future differentiators for providers in the healthcare market.
Unfortunately, one of the primary challenges of delivering on this definition of digital health is a lack of interoperability and integration both within and between healthcare organizations, which means that data cannot be leveraged to maximize its value. It’s not just enough to have astronomical amounts of data; it has to be delivered to the right person at the right time.
A combination of limited funding and a conservative approach to technology seem to be the biggest obstacles to the adoption of digital health in Ontario, but Laurie Poole is optimistic: “Technology used to be an afterthought, so there has been a big shift from even four years ago.”
However, funding models that reward physical presence rather than virtual care, and privacy legislation that limits how organizations store and share data are two big barriers noted by David Denov and Dr. Jamieson. “Hospitals and providers have convinced themselves that change has to be incremental, and that disruption is undesirable,” says Dr. Jamieson. “You will never have innovation without a bit of risk.” Clearly innovation needs to be balanced with the risk and potential consequences for patients and their data.
Looking to other health systems that have achieved widespread adoption of technology and digital health, it appears that that big changes have to be driven (or at least strongly supported) from the top down – and not just within the hospital, but from health systems or regional leadership in healthcare. Poole points out that integrated health systems in the US have leveraged their power as a closed system with a single HIS to drive mainstream adoption of virtual care, but that a lack of integration in Ontario has been a key challenge in achieving the same adoption. Many G8 countries are facing similar challenges of constricted spending, limited infrastructure and an aging population, and consolidating leadership at a regional or provincial level may help coordinate adoption. “Every [Ontario] hospital has an independent board of directors,” Dr. Jamieson adds, which may contribute to the challenges in achieving widespread adoption.
This might imply that Ontario hospitals are stuck in siloed information systems without a strong mandate from provincial leadership, but momentum is building and there are a number of initiatives which are working towards broader integration. Initiatives such as ConnectingGTA and the current [as of 2016] provincial hold on new Hospital Information System implementations may be the first step towards standardization.
From the patient perspective, there is a growing expectation of digital health integration throughout their healthcare journey regardless of care location. Many of our Ontario hospitals have been able to leverage digital health effectively within their own organizations and work with healthcare partners on a community level, but growing pressure from patients will likely continue to push for provincial and even national initiatives which improve on inter-organizational integration. It is certainly clear that digital health has the opportunity to transform how care is delivered to the patient – from improved data analytics & big data to driving better patient outcomes through 360-degree healthcare coordination, digital health is becoming an essential part of effective healthcare.
Author: Kim Osborne Rodriguez, P.Eng., RCDD

The information technology needs of health care institutions are rapidly expanding, which makes it critical that the communications infrastructure is planned strategically.
Authors: Kim Osborne Rodriguez, P.Eng., RCDD | Megan Angus, RN, MBA, Lean, EDAC
Published September 2015 in the Canadian Consulting Engineer Magazine
Download complete article - Future-Proofing Hospitals – September 2015 >

You might have heard about some new technologies in healthcare and other industries lately, or had colleagues ask about technologies they’ve heard of or seen in other hospitals. The Angus Connect group helps our clients understand and evaluate these technologies to identify those which provide the best value and strategically align with the goals of the hospital, then assist with planning and specifying the implementation of the selected systems. Click to Download complete Article >
Author: Kim Osborne Rodriguez, P.Eng., RCDD