British Columbia's first fully electric healthcare facility has achieved Zero Carbon Building - Design Standard™ certification from the Canada Green Building Council. This is the first hospital in Canada to achieve this certification. The Standard guides the design of new buildings and major renovations of existing ones so they can achieve zero carbon operations. Environmentally sustainable hospital design delivers benefits for healthcare operators, patients and healthcare staff, and the communities they serve.
The Zero Carbon Building (ZCB) - Design Standard™ defines low-carbon design and operational performance for buildings. According to CaGBC’s website, “The Zero Carbon Building – Design Standard™ guides the design of new buildings and major renovations of existing ones so they can achieve zero carbon operations. The Standard is comprehensive and evaluates the anticipated carbon emissions from building operations like heating and cooling. Project teams must carefully consider the embodied carbon of construction materials, refrigerants used in HVAC equipment, and building airtightness. Project teams must also evaluate strategies to minimize electrical grid impacts."
The Project
HH Angus is providing mechanical and electrical consulting engineering to the Cowichan District Hospital Replacement Project (CDHRP) on Vancouver Island, as part of the design team under the Nuts'a'maat Alliance (Island Health, EllisDon Corporation, Parkin Architects, BC Infrastructure Benefits and Infrastructure BC). The project is being developed for Island Health to replace the existing facility in North Cowichan, BC. When it opens in 2027, the new hospital will be three times larger than the existing facility at 57,448 m2 (607,601 ft2), and will increase capacity from 148 beds to 204 beds. The hospital will expand capacity for inpatient and ambulatory care, with seven operating rooms, additional procedure rooms, an expanded birthing unit, pediatric spaces, outpatient clinic services, expanded diagnostic imaging, an expanded emergency department, and a rooftop helipad. Mental health services will be updated with a 20-bed inpatient psychiatry unit and a four-bed psychiatric intensive care unit.
Sustainability Features
Sustainability has been at the core of the decision-making process for this project, with a focus on carbon reduction. Its ZCB – Design™ certification reflects achieving a 38% embodied carbon reduction from baseline and, as the first all-electric healthcare facility in British Columbia, the CDHRP’s design has an operational energy performance that significantly surpasses its target.
The design strategies focused on reducing the project's embodied carbon emissions, maximizing energy efficiency, electrifying the mechanical systems, using new-generation low GWP refrigerants, and designing an optimized PV array.
In its press release announcing the ZCB – Design™ certification, Island Health provided the following highlights of the hospital features supporting patient and staff wellbeing and environmental benefits:
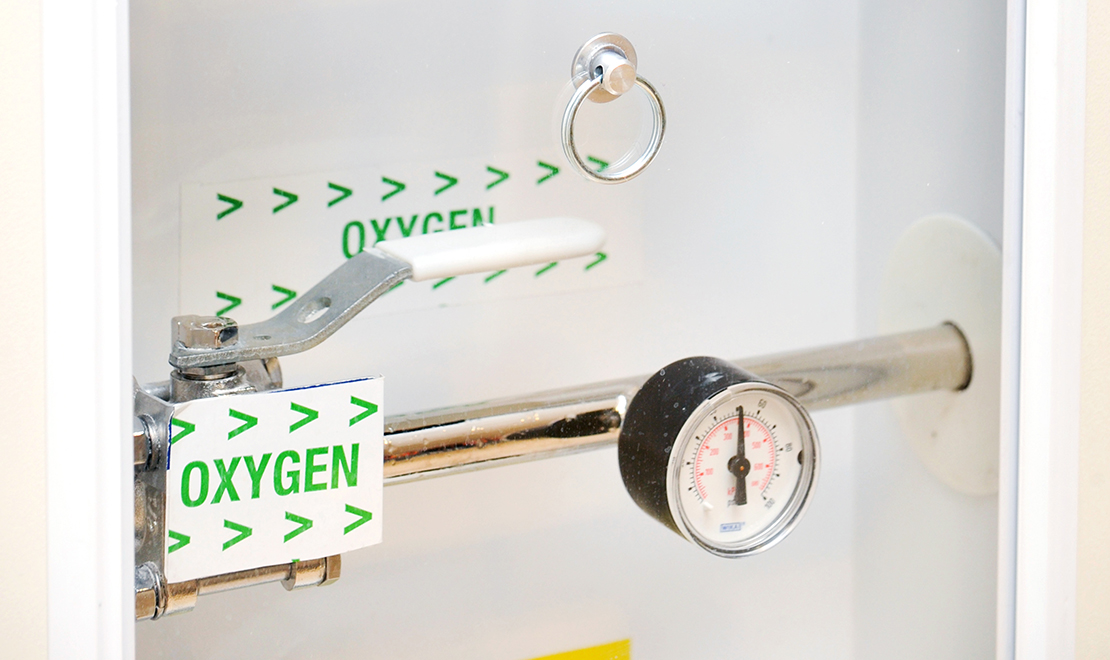
- Fully electric operation: The first all-electric hospital in B.C., it eliminates reliance on fossil fuels.
- Highly energy efficient design: A high-performance building envelope minimizes heat loss, reducing overall energy demand by 30% compared to the current hospital.
- Better air quality: Advanced ventilation and filtration systems support cleaner air, benefiting people with respiratory conditions such as asthma and COPD and providing greater operational resilience during wildfire smoke events.
- On-site renewable energy generation: Rooftop solar panels will generate 2.5 percent of the hospital’s annual energy needs, reducing operating costs and reliance on external energy sources.
- Water conservation strategies: 60% more water-efficient than the current hospital
- Sustainable materials: Use of low-carbon concrete, mass timber, rebar and insulation to minimize embodied carbon in construction.
- LED lighting which uses 75 percent less energy than incandescent bulbs; and
- Low global warming potential refrigerants to minimize carbon emissions in mechanical equipment.
The EllisDon and Parkin-led (ED+P) design team, in association with HH Angus, ZGF Architects, Bush Bohlman and Partners, and RDH, understood the significance of the project goals and the importance of targeting the Zero Carbon Building – Design™ certification. Their leadership, efforts and collaboration allowed the team to meet and exceed the project requirements, together with the leadership of Island Health. The project team members have been consistently committed to following through on the design approach and to finding all opportunities to improve.
To view a short video about the project’s construction progress, click here.
To read more about our work on the Cowichan District Hospital Replacement project, click here.
Image/s courtesy of EllisDon Construction & Parkin Architects