Isolation Room Design Criteria
Key room design factors include high level air separation (7.5 Pa of negative or positive pressure, 12 air changes per hour and directional airflow, with non-aspirating diffusers and low-level exhaust near the head of the patient bed.) Also required: a higher level of airtightness to maintain pressure, and consideration of pressure testing during construction to verify effectiveness.
An important tip: during construction, ensure contractors clearly understand what the room will be used for, why sealing is so critical, and why it is vital that there be no leakage.
Regarding ‘grandfathering’ of existing rooms - these require a risk assessment to identify any deficiencies that must be addressed in order to meet the revised standard. Some common leakage sources include lighting fixtures, conduits, sliding doors and uneven floors.
Redundancy
Isolation rooms are designated as a Type 1 space under CSA HVAC standards, requiring uninterrupted operation for airflow, pressurization, temperature, exhaust systems for AIRs, and supply systems for PERs. AHUs require redundancy with parallel, interconnected systems with automated controls and emergency power.
Filtration
AIR supply air requires two-stage filtration. PER and combination AIR/PER supply air requires three-stage filtration, with HEPA filters downstream of MERV 8 and MERV 14 filtration. HEPA filters can be AHU mounted, duct mounted or terminal. All require accessible means of testing. On the exhaust side, AIR and AIR/PER exhaust air is treated as contaminated exhaust, and must comply with CSA Z317.2 requirements. Additionally, recent design improvements for contaminated exhaust include bag-in/bag-out HEPA filters on the exhaust system, in order to reduce the potential for outdoor wind, building wake zones and surrounding buildings to disperse contaminated air.
Anterooms
Anterooms are now required for all AIRs, per Z8000-18, to offer additional controls against unwanted air movement, and for the donning and removal of PPE, among other considerations. Air flow should be negative relative to the corridor and positive relative to the isolation room. Also required – dedicated exhaust from both patient room and anteroom, with the adjacent washroom connected to the dedicated exhaust.
Studies provide strong evidence supporting the use of anterooms, due to the re-emergence of infectious diseases, such as tuberculosis. The CSA has completed a research study of pressure differentials, which interested readers may benefit from consulting: “Pressure Differential in Health Care Facility Airborne Isolation Rooms”. The study, a comprehensive examination of available literature, is helping to inform CSA standards, as well as zoning for pandemic requirements. For example, one finding is that anterooms provide significantly improved containment of particles at pressure differentials above 2.5 Pa, especially during healthcare provider movement through doors. Other systems proven effective in augmenting traditional cleaning are ultraviolet germicidal irradiation systems (UVGI).
Pandemic Planning and Catastrophic Event Management
Designing for planning and management of pandemic and catastrophic events requires consideration of zoning, and how healthcare facilities can isolate entire areas of a healthcare facility. As well, the facility will need the ability to switch between 100% outdoor air to 100% recirculated air, depending on where contaminants originate. Negative pressure ‘pods’ for ERs and ICUs are also a design consideration, providing the ability to lock down larger areas of a hospital.
Outbreak Control Zone
These zones have already been in place in British Columbia for the past 12 years, primarily in inpatient areas and ICUs. To create an isolation pod, a typical 16-bed unit is identified and planned as an outbreak control zone. It is designed as a standard patient care unit, but one that can be self-contained. Within the walls of the unit, allowances have been made for clean and soiled holding areas in order to reduce traffic in and out of the control zone. In addition, the area design should provide for a relatively simple procedure to convert it to negative pressure. Also required are defined space for an anteroom that meets the standards for whole unit isolation with all air being exhausted, as well as pressure monitoring and alarms. In addition, controls must be programmed into the Building Management System at the required isolation unit settings, in order to provide single command implementation. These systems are then commissioned, balanced and demonstrated to the facility as part of the verification process.
Operations and Maintenance
CSA Z8001 Commissioning and CSA Z8002 Operation and Maintenance (O&M) standards both offer useful information for O&M processes. Some design considerations to facilitate O&M are: including accommodations for testing and precautions for those who will need to provide O&M for isolation rooms; accessible locations for safely changing bag-in/bag-out HEPA filters; servicing for ductwork inspection and cleaning (annually for CSA and semi-annually for MOL).
Of special note: isolation rooms tend to lose pressure over time. For HVAC performance, this stems from degradation of doors and frames, wall openings for maintenance work that were subsequently not properly sealed, damage to walls, and poor sealing of services penetrating walls above ceilings.
Reactivation, Conversion and Retrofits
During the current COVID-19 pandemic, hospitals are seeking to better protect healthcare workers from getting sick, as well as looking at options for safe and fast reactivation of medical and surgical beds to respond to increased demand, including conversions/retrofits of hospital infrastructure to enable this reactivation.
Other options for some healthcare facilities may involve identifying beds/units that were initially designed to serve as AIRs, but were since repurposed. These would require detailed inspection and testing, along with any attendant servicing to ensure the rooms/units meet all relevant codes and standards for patient and staff safety.
In identifying potential conversion space, hospitals should look for an existing patient area where access to the area can be controlled to minimize interaction between COVID-19 patients and healthcare staff/other patients. The space should also have the ability to be converted to outside air/exhaust that can enable a slightly negative pressure condition relative to the adjacent space which helps in controlling the spread of infectious germs from patients throughout the area. Alternatively, consider modifying an existing private room(s) with individual ductless units which do not circulate through ductwork into a central HVAC system.
For any AIR, the key is to control airflow to manage all contaminants, whether gases or droplets. The air handling strategy utilized (mixed ventilation, displacement ventilation or other) will depend on the size of the room, layout and other factors.
Because speed of construction and becoming operational is critical, effective collaboration and trust between hospital administrators, engineers, designers and contractors is essential. The entire team has to get these rooms designed, approved, built and operating quickly.
Guidance Documents
Canadian Standards Authority guidance documents dealing with standards for isolation rooms include:
CSA Z8000 Canadian health care facilities | latest issue 2018
CSA Z317.2 Special requirements for HVAC systems in health care facilities
CSA Z317.1 Plumbing
CSA Z317.13 Infection Control
CSA Z317.12 Cleaning and Disinfection – coming soon
Cancer Care Ontario Position Statement – Hospital isolation practices for hematopoietic stem cell transplantation
CSA Study Executive Summary:
Pressure Differential in Health Care Facility Airborne Isolation Rooms
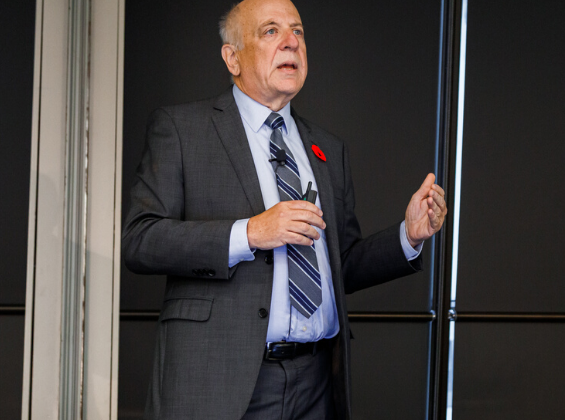
Advisory Panel members include HH Angus’ Nick Stark and Rita Patel